An outbreak begins in one part of the world: is it a natural outbreak or the result of an act of bioterrorism? And after all: is it really important to differentiate?
An excellent article by Lionel Koch et al (1) of the IRBA, published in 2020, provides an overview.
What is it about?
The COVID-19 epidemic has challenged the entire scientific community. Even the oldest among us have not experienced an outbreak of this magnitude, the last one being the influenza pandemic of 1918-19, which caused more than 60 million deaths on all continents. Under these conditions, it is quite understandable that the reaction of the public authorities was difficult to carry out, even with the advice of an enlightened “scientific council”.
Moreover, the revelation of the different biological warfare programs developed by different countries, such as the Gruinard Island [1] experiments carried out by the British (1942-43), the American program begun in 1942 at Fort Detrick [2] (Maryland), the Soviet Biopreparat [3]program (from 1972), the Japanese Unit 731 [4] program (1932-1945), and the Iraqi program (1985-1991) with the production of 8,000 liters of B. anthracis suspension, can make us fear that such an epidemic could be the result of a state bioterrorism, or of a terrorism attributable to more restricted groups such as the Aum sect (in April 1990, members of the sect spread botulinum toxin aerosols in the streets of Tokyo and Yokohama) and or the American Rajneeshees. [5]
Let’s ask ourselves the question? Is it really necessary to quickly distinguish between the natural or bioterrorist origin of an outbreak, especially when it spreads rapidly to become a pandemic?
Emerging infectious disease outbreaks
The globalization of international trade contributes to the inefficiency of common quarantine measures to contain the disease and this is why the rate of these epidemics has increased in the last 30 years:
SARS epidemic (SARS Cov), 774 deaths, 2002-2004, worldwide
Ebola epidemic in 2013-2016 (11,310 deaths) in West Africa that has been considered a paradigm of the problems caused by emerging infectious diseases today. Indeed, this fearsome pathogen naturally emerged in a new, vast area, and its spread that nothing seemed to stop then impacted Europe and the United States.
The SARS-Cov-2 outbreak followed the same pattern.
Monkeypox 2022, it spreads in the world but its mortality remains low.
Thus, outbreaks can no longer be seen as local and distant problems, but must be addressed on a global scale.
Nowadays, when an outbreak occurs, it seems that one of the first concerns of the authorities is to distinguish a natural outbreak from an intentional act involving a biological threat agent in order to better adapt their management. Even SARS-CoV-2 has not escaped the suspicion that it was engineered in a laboratory (2).
Natural or provoked outbreak: how to distinguish them?
The simplest reason to look for the origin of an outbreak could be the application of the Biological Weapons Convention, signed in 1972, which prohibits the use of biological weapons (3). The identification of a biological attack then becomes a major international political and judicial issue.
But the evolution of a natural outbreak depends on a large number of interrelated factors such as climate change, natural disasters, human actions…
Is the rare nature of the infectious agent synonymous with a terrorist act?
- Yes, in the case of the strain of Bacillus anthracis used in the letters addressed to political figures during the 2001 attacks in the US (attack also called Amerithrax);
- Yes, in the case of the strain of Bacillus anthracis used by the Aum sect in 1993 and sprayed on Kameido;
- No in the case of Ebola in the 2014-15 outbreak;
- No in the case of the 2017 outbreak of pneumonic plague (Yersinia pestis) in Madagascar.
- Counter-example: the Rajneesh cult intentionally used a common strain of Salmonella to poison salads in several Wasco County bars in an attempt to neutralize the voting population in the town of The Dalles so that their own candidates would win the 1984 Wasco County election.
Spatial and temporal distribution?
Spatial distribution
If a pathogen is detected in a place where it has never been detected before, could this be an indication of suspected biological attack?
- Yes, as happened during the Amerithrax crisis in 2001, when a Texas strain of B. anthracis was discovered on the east coast of the US.
- No, because the largest outbreak of Ebola occurred in a part of the continent previously recognized as free of the disease!
Seasonality
If an outbreak occurs during a season that is incompatible with the life span of the pathogen, could human activity be blamed? No, with the example of the H1N1 pandemic in 2009, which appeared in April in North America with two outbreak peaks, and which emerged in an unusual way from infected pig populations, followed by a unique global spread!
The origins and dynamics?
Can multiple starting points usually mean a biological attack?
- Yes for the five mailings containing B. anthracis spores in the US and the many restaurants targeted by the Rajneesh cult;
- No, as with that natural tularemia outbreak in Kosovo in 1999-2000 that reached several districts simultaneously in a tense geopolitical context and, in 2017, during the plague outbreak in Madagascar that had multiple index cases.
Could an unusually rapid spread or a large portion of the population quickly affected be evidence of a biological attack?
- No. SARS-CoV 2003 and SARS-CoV-2 spread very rapidly throughout the world, with more than 200 countries affected in one year for the former and 30 countries in 5 months for the latter, although they are natural outbreaks.
Is there any value in identifying one from the other?
The confusion surrounding the criteria for differentiation confirms that the two phenomena are intimately linked.
The real challenge for global security remains early detection, accurate characterization, and implementation of specific measures, regardless of the origin of the outbreak. During the COVID-19 crisis, it was felt that early detection and isolation of cases would have been more effective in preventing infection than travel restrictions and contact reduction.
Early detection
Some diseases, such as influenza, are monitored internationally, while others are actively monitored in the context of an outbreak, such as the Ebola virus in the last outbreak in West Africa. For these well-known diseases, the definition of cases is clear and an outbreak is declared when the number of cases exceeds a certain threshold. This classic method requires an expensive and complex public health network and the alert is often activated with some delay.
In the case of new diseases or conditions with polymorphic or non-specific symptoms, the definition of cases and the threshold for reporting the outbreak are subject to debate.
Systematic environmental monitoring for all diseases is, at present, impossible due to technological barriers and cost issues.
However, there are a number of possibilities, such as sewage testing, which could be a good way to monitor the spread of SARS-CoV-2 in the community.
The role of health workers is essential because they are the first to observe an unusual event (new disease or increased number of cases): they must be able to warn public health officials. To do so, they must be trained and know how to use computerized epidemiological surveillance tools.
The use of social networks can also be a powerful means of data collection but there are many biases such as the fear generated by the disaster scenario of a movie for example.
The monitoring of vital parameters such as temperature and heart rate of individuals connected to their smartphone, coupled with their geolocation can also be a good way to detect abnormal events. Other systems such as video surveillance already used in China could also serve as an alert. The analysis of the results can only be done with the assistance of powerful artificial intelligence systems. Personally, I think that these systems are still in the realm of utopia, if only because they involve the use of personal data! The simple use of the “#TousAntiCovid” application has shown us how difficult it is.
Crisis management
Early detection is critical, but it must be followed by the resources needed to deal with the crisis. Infrastructure, PPE (remember the sad story of the lack of masks at the beginning of Covid and which endangered the entire health system!) must be ready. The coordination of civil, military, governmental and non-governmental emergency plans must have been exercised beforehand. Global coordination in the case of pandemics should also be planned.
For a health care system, preparing for a biological attack or a natural outbreak is broadly the same challenge. In addition, preparedness for biological attacks has significant added value in enhancing preparedness for natural outbreaks, and vice versa.
It is therefore economically attractive to consider the natural biological risk and the possibility of an attack as a single threat in preparing the response to an infectious event with outbreak potential. The crisis generated by the many deaths from COVID-19 and the containment of billions of people could probably trigger a new evaluation of public policies for controlling outbreaks, with the opportunity for public opinion to take a fresh look.
Conclusion
Thus, we have just seen that there is no easy way to distinguish a natural origin from a bioterrorist origin, but they have the same consequences and should have a common management. Therefore, pooling preparedness measures and response tools against both the emergence of an unknown pathogen and an unpredictable attack will maximize the effectiveness of the response.
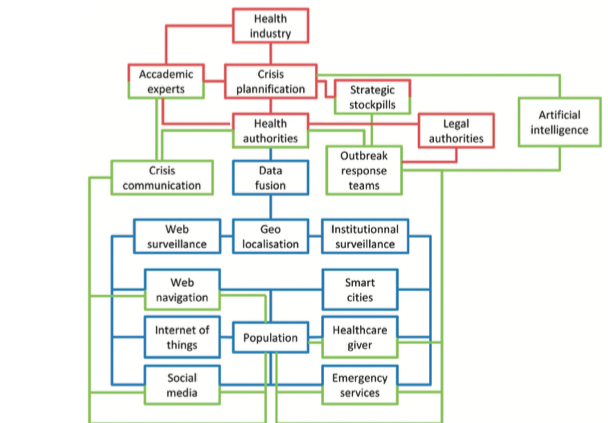
To summarize: whatever the origin, natural or bioterrorist, of an outbreak, the means to be implemented to face it efficiently include a quick and efficient detection involving a systematic surveillance of infectious phenomena by means of AI, a passage of information (in particular social networks), followed by a no less efficient crisis management previously prepared including infrastructures, PPE, and the coordination of the different services
The key concepts are therefore communication (regional, national and global networks) and artificial intelligence (detection and crisis management).
Nevertheless, determining the origin is important in order to prosecute possible violators of the 1972 Biological Weapons Convention and/or to better understand the natural emergence of a germ with a particular pathogenicity, to follow its evolution to other forms and to monitor its appearance in other parts of the world.
References
- Koch L., Lopes A.A, Maiguy A., Guillier S., Guillier L., Tournier J.-N, Fabrice Biot F, Natural outbreaks and bioterrorism: How to deal with the two sides of the same coin? www.jogh.org doi: 10.7189/jogh.10.020317
- Hao P, Zhong W, Song S, Fan S, Li X. Is SARS-CoV-2 originated from laboratory? A rebuttal to the claim of formation via laboratory recombination. Emerg Microbes Infect. 2020;9:545-7. Medline:32148173 doi:10.1080/22221751.2020.17 38279
- Feakes D.The Biological Weapons Convention. Rev – Off Int Epizoot. 2017;36:621-8. Medline:30152458 doi:10.20506/ rst.36.2.2679