Sarin gas was developed in 1939 in the laboratories of IF Farben. Sarin stands for Schrader, Ambros, Rüdiger and Van der Linde, named after the inventors who gave it their initials.
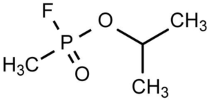
It belongs to the organophosphorus family, which includes agents such as insecticides and also warfare agents such as G agents: GA tubun, GB sarin, GD soman, V agents: VX and VR and A agents also known as Novitchok agents (agents A-230, A-232 and A-234). An assassination attempt on Alexei Navalny in 2020 was carried out by an A agent.
Acetylcholine (ACh) is a neuromediator that plays a role in both the central nervous system (memory, learning) and the peripheral nervous system (muscle activity and vegetative functions).
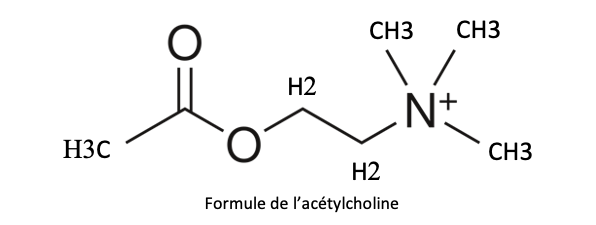
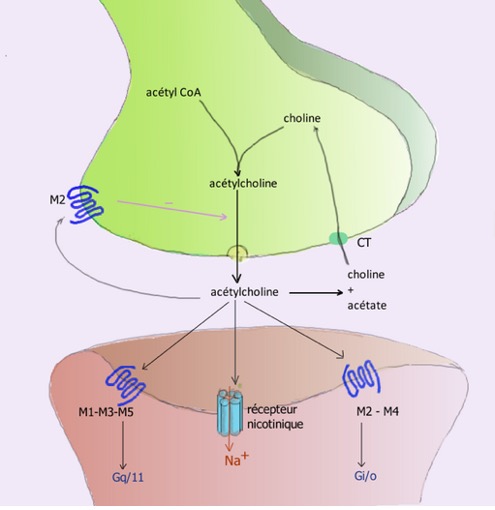
In a neuron, acetylcholine is stored in the vesicles of the presynaptic membrane (remember, a synapse is the zone between the end of a neuron and either another neuron or a muscle cell). When an action potential arrives at the tip of the neuron, it causes Ca++ channels to open, resulting in vesicle fusion and the release of ACh into the synaptic cleft. It then reaches the postsynaptic receptors (i.e. on the other side of the gap) and causes a change in membrane ionic permeability and muscle contraction if it’s a neuromuscular junction.
There are 2 types of receptor: muscarinic receptors, divided into 5 classes from M1 to M5, and neuronal N1 nicotinic receptors (central nervous system, peripheral ganglia and muscular ganglia), and muscular N2 nicotinic receptors.
| Tissu | Effect of acetylcholine | Receptors involved |
| Nervous system | Memorization and learning | M1 |
| Heart | Decreased heart rate | M2 |
| Vascular | Vasodilation, lower blood pressure | M3 |
| Lung | Bronchial contraction, secretion | M3 |
| Intestines, Stomach | Contractions, secretions | M3 |
| Salivary glands | Secretion | M3 |
| Eye | Pupil contraction, tears | M3 |
| Adrenal gland | Inhibits adrenalin secretion (no longer stimulated by the orthosympathetic system) | N |
| skeletal muscle | Contraction | N |
In all cases, ACh must be rapidly removed from the synapse after release, and to do this it is hydrolyzed by an enzyme, acetylcholinesterase (AChe), into acetate and choline in just a few milliseconds.
Acetylcholinesterase inhibitors
In the medical field
In certain diseases, it is necessary to increase cholinergic transmission, for example by providing (non-hydrolysable) cholinergic receptor agonists (muscarine, alkaloids, nicotine…). Acetylcholinesterase inhibitors such as physostigmine and pyrodostigmine can also be used, and various other inhibitors are being tested to treat the cholinergic deficiencies associated with Alzheimer’s disease (rivastigmine, etc.).
More specifically, ACh receptor antagonists such as belladonna and atropine can also be used.
Organophosphorus
These neurotoxic organophosphorus molecules block acetylcholinesterase (AChE).
This is the case with Sarin.
By blocking acetylocholinesterase, acetylcholine accumulates at synapses and over-stimulates nerves, muscles and glands (notably the lacrimal glands), salivary glands and sweat glands throughout the body. Stimulated muscles initially tremble and contract uncontrollably, then fatigue and weaken.
Exposure to nerve agents can lead to long-term neurological and neurobehavioral disorders, including anxiety, depression, irritability and memory problems. (MSD)
Organophosphorus (OP) mode of action
They bind to any cholinesterase and phosphorylate the esterase site of the enzyme, thus preventing the physiological hydrolysis of acetylcholine to choline and acetic acid. Dephosphorylation of the OP-inhibited enzyme is very slow, but can be accelerated by a cholinesterase reactivator or “oxime”, part of the current treatment of intoxication.
At room temperature, sarin is a liquid that evaporates easily, attacking the individual via the cutaneous and respiratory routes. Exposure of the skin to these agents initially causes contractions and sweating at the site of exposure. Whole-body effects occur after a delay of up to 18 hours following exposure to a G or V agent.
Nerve agents stimulate nerve cells in the brain, causing people to become agitated, confused, prone to convulsive seizures or unconsciousness.
Stimulation of nerve cells outside the brain causes nausea, vomiting, tears, nasal secretions, heavy salivation, lung secretions, wheezing, exaggerated digestive secretions (such as diarrhea and vomiting), and sweating. Stimulation of muscle cells leads to cramping, followed by weakness and paralysis. Weakness of the respiratory muscles and interruption of the respiratory center in the brain are usually the cause of death.
Diagnosis in the field is carried out by a physician, based on the history of the area, the toxidrome and the use of paper detectors, or other types of detectors.
Treatment
- Symptomatic treatment is essentially respiratory resuscitation. This is based on various measures to open the airways and provide oxygen therapy, including intubation and controlled ventilation. Its effectiveness is well established, but limited in the event of massive influx.
- The essential anticonvulsant treatment relies on benzodiazepines (Valium) and, more recently, ketamine.
- Two drugs are usually administered: atropine and pralidoxime.
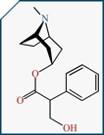
Atropine
Atropine is the true antidote to OP intoxication. Atropine competes with acetylcholine at muscarinic receptors, but has no effect on cholinesterases at the neuromuscular junction. Atropine blocks ACh receptors, preventing ACh from further stimulating neurons. Pralidoxime is a cholinesterase reactivator which not only hydrolyzes the enzyme-inhibitor bond, but also the inhibitor, acting synergistically with atropine to reduce the latter’s dose. It binds to the alkyl-phosphate group of alkyl-phosphorylated cholinesterase and detaches it from acetyl-cholinesterase, which is thus regenerated.
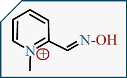
Pralidoxime
Auto-injectors containing both products are available.
Phosphorylation of cholinesterase
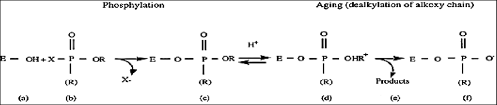
Illustration of the phosphorylation and aging mechanism of cholinesterase. (a) free enzyme; ( b) organophosphorus compound; (c) phosphorylated enzyme; (d) intermediate; (e) dealkylation products and (f) aged enzyme..
Pralidoxime mode of action: reactivation of cholinesterase
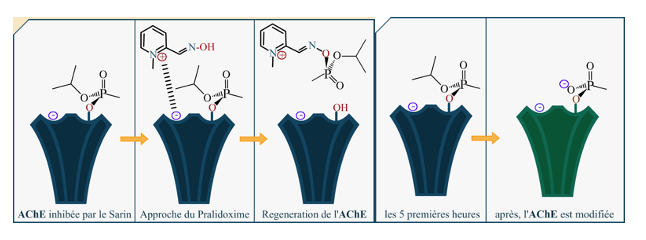
Pralidoxime’s mode of action is no longer valid if exposure to Sarin exceeds 5 hours. This is the result of a long-term AChE aging process, also known as the “Aging Porcess”.
AChE aging process after 5 hours’ exposure to Sarin – deteriorated AChE (here in green)
These highly instructive figures are taken from the article on Sarin in the magazine “Zeste de savoir“.
Decontammination
It reduces the dose of organophosphorus absorbed through the skin, preventing contamination transfer to the surrounding area (DecPol Abs). In the event of a chemical alert, the nature of the toxic agent, which is often unknown, increases the number of potential victims, with a major risk of contamination transfer (see the situation of healthcare workers during the sarin gas attack in the Tokyo subway).
Sarin uses
In a previous article, we reported on the many uses of sarin gas, both by terrorists and by governments. It’s worth reminding ourselves that this product has been widely used.
Going a step further: Gulf War Syndrome
Reports on “Gulf War Syndrome” have led to speculation on possible associations between toxic exposures.
Depleted uranium was not selected as a cause, leaving exposure to aerosolized organophosphate compounds (pesticides and the nerve agent sarin) as the most likely cause(s) of Gulf War Syndrome.
In an interesting study by H.M. Bolt, the question was raised whether Sarin might have played a role in Gulf War Syndrome.
The study of the genetic polymorphism of the paraoxonase-1 (PON1) Q192R genotype may provide information on its association with certain conditions or diseases, including metabolic disorders such as type 2 diabetes, obesity, or other cardiovascular diseases.
In our case, we wanted to find out whether Gulf War Syndrome is related to exposure to low doses of nerve agents?
The study was carried out on 508 sick soldiers compared with 508 non-sick control soldiers.
Exposure to low doses of nerve agents was estimated using survey questions about having heard audible nerve agent alarms in the field.
Studies showed that the gene-environment interaction of the Q192R genotype and auditory alarms was strongly associated with Gulf War illness.
All in all, these data support the idea of a causal relationship between low-level organophosphorus compounds, particularly sarin, and the symptoms of Gulf War illness. In the lay press, speculations have been made about a link with the bombing of Sadam Hussein’s chemical weapons cache in January 1991 around the towns of Muthanna and Fallujah, which had released sarin.
Conclusion
Given the complexity of sarin’s systemic toxic actions, particularly those affecting the brain, and the absence of effective antidotes against damage to the Central Nervous System, research into sarin’s toxicity may continue for a long time to come.
References
- Hermann M. Bolt, Sarin: a never‑ending story, Archives of Toxicology, on line 28 nov 2022
- Intoxications par les organophosphorés Consensus d’actualisation SFAR – Médecine d’urgence 1999 J.M. Saïssy, M. Rüttimann
- Acétylcholine, Wikipédia, consulté le 3 mars 2024
- UA Okoli, NI Nubila and MT Okafor, Organophosphorous Pesticide: An Environmental Pollutant Perspective, Journal of Chemical and Pharmaceutical Research, 2017, 9(9):126-130
Autor: Prof. François Renaud



